ARE YOU A HEALTHCARE PROFESSIONAL?
This site is intended for US healthcare professionals only.
By clicking YES, you attest that you are a healthcare professional licensed in the US.

Dysport is not interchangeable with other botulinum toxins, and the potency units are not the same1
Units of biological activity of Dysport cannot be compared to, or converted into, units of any other botulinum toxin product
Dysport has clear dosing guidelines and a dosing app to help you inject approved muscles with appropriate doses1
Dosing is based on Dysport Units per kilogram of body weight1
Convert from pounds to kilograms (1 kg is equal to 2.2 lb)
Prioritization of muscles may be required to stay within the recommended dose range.
Recommended total UPPER LIMB SPASTICITY Dysport dose per treatment session:
Recommended total LOWER LIMB SPASTICITY Dysport dose per treatment session:
In pediatric patients treated for BOTH UPPER AND LOWER LIMB SPASTICITY:
The total dose administered should be divided between the affected spastic muscles.1
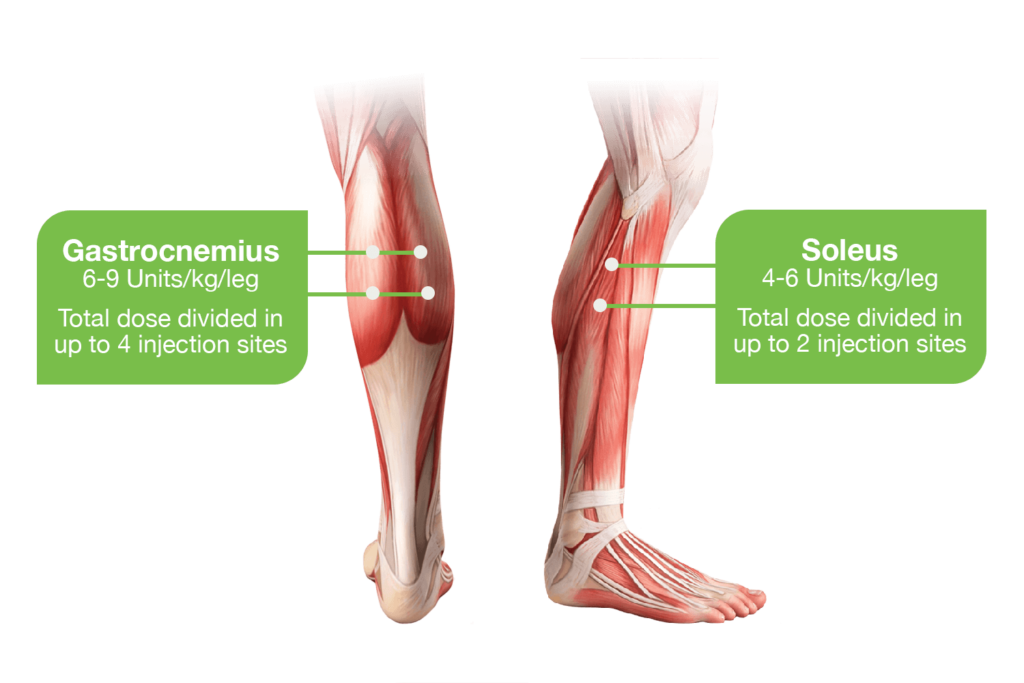
When possible, the dose should be divided across more than 1 injection site in any single muscle.
No more than 0.5 mL should generally be administered at any single injection site; although actual location of the injection sites can be determined by palpation, the use of injection guiding technique, eg, electromyography or electrical stimulation, is recommended to target the injection sites
Dosing in initial and subsequent treatment sessions should be tailored to the individual based on1
Retreatment
*Patients who remained in the upper limb study after week 16 were permitted additional discretionary follow-up visits at week 22, week 28, week 34, or beyond.3
†Patients who remained in the lower limb study after week 12 were permitted additional discretionary follow-up visits at week 16, week 22, and week 28 to assess eligibility for retreatment.3
FDA-approved doses range and muscles for injection for pediatric patients with upper limb spasticity or lower limb spasticity
Muscles for injection for upper limb spasticity in pediatric patients with their respective FDA-approved Dysport dose range.

Muscles for injection for lower limb spasticity in pediatric patients with their respective FDA-approved Dysport dose range.
Considerations for achieving desired concentration include: the patient’s weight, limit of 0.5 mL per injection site, the recommended number of injection sites per muscle.
For other dilution options, refer to Table 1: Dilution Instructions for Dysport Vials (500 and 300 Units) in package insert Section 2.2: Preparation of Dysport Solution for Administration
Examples of dilutions with Dysport 300-Unit and 500-Unit vials
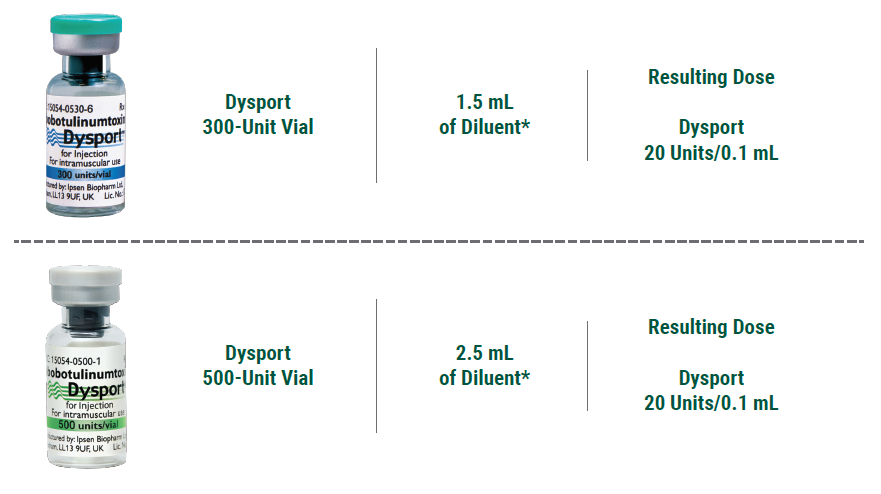
Other dilutions may be necessary to enable dosing flexibility; for example:
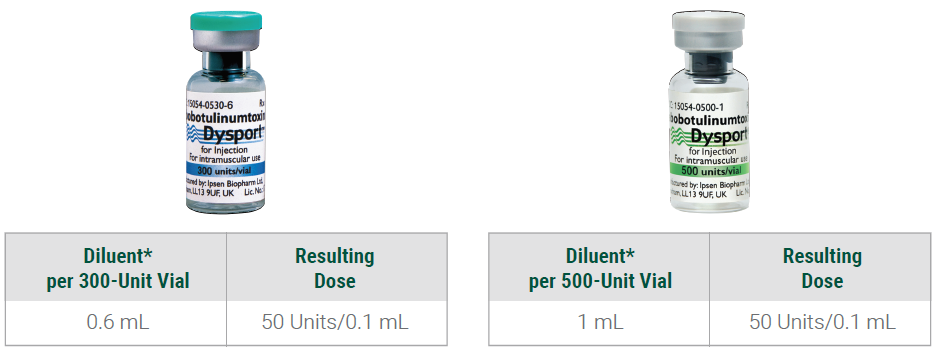
Adapted from Section 2.2, Table 1 of the Full Prescribing Information.
*Sterile, preservative-free 0.9% Sodium Chloride Injection, USP.
Reconstituted Dysport is for intramuscular injection only.
Recommended Doses
*Sterile, preservative-free 0.9% Sodium Chloride Injection, USP
Reconstitution instructions are specific for the 300-Unit and 500-Unit vials.
Reconstituted Dysport is for intramuscular injection only.
Dilution & Reconstitution
C.L.I.M.B. is a multitier learning continuum designed to accommodate physicians new to and experienced with botulinum toxin therapy. This educational curriculum is designed to help physicians across all levels improve their clinical skills involving the appropriate use of Dysport through online e-learning modules discussing some of the latest advances in the field for diagnosis, treatment and outcomes, on-demand peer-to-peer programs, and other educational resources. Be sure to visit CLIMB-training.com often to check for new content and updates.
E-learning modules currently available for adult spasticity.
Training
Postmarketing reports indicate that the effects of Dysport and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence, and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity, but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses and in approved indications, cases of spread of effect have been reported at doses comparable to or lower than the maximum recommended total dose.
Dysport is contraindicated in patients with known hypersensitivity to any botulinum toxin products, cow’s milk protein, components in the formulation or infection at the injection site(s). Serious hypersensitivity reactions including anaphylaxis, serum sickness, urticaria, soft tissue edema, and dyspnea have been reported. If such a reaction occurs, discontinue Dysport and institute appropriate medical therapy immediately.
Lack of Interchangeability Between Botulinum Toxin Products
The potency Units of Dysport are specific to the preparation and assay method utilized. They are not interchangeable with other preparations of botulinum toxin products, and, therefore, units of biological activity of Dysport cannot be compared to or converted into units of any other botulinum toxin products assessed with any other specific assay method.
Dysphagia and Breathing Difficulties
Treatment with Dysport and other botulinum toxin products can result in swallowing or breathing difficulties. Patients with pre-existing swallowing or breathing difficulties may be more susceptible to these complications. In most cases, this is a consequence of weakening of muscles in the area of injection that are involved in breathing or swallowing. When distant side effects occur, additional respiratory muscles may be involved. Deaths as a complication of severe dysphagia have been reported after treatment with botulinum toxin. Dysphagia may persist for several weeks, and require use of a feeding tube to maintain adequate nutrition and hydration. Aspiration may result from severe dysphagia and is a particular risk when treating patients in whom swallowing or respiratory function is already compromised. Patients treated with botulinum toxin may require immediate medical attention should they develop problems with swallowing, speech, or respiratory disorders. These reactions can occur within hours to weeks after injection with botulinum toxin.
Pre-existing Neuromuscular Disorders
Individuals with peripheral motor neuropathic diseases, amyotrophic lateral sclerosis, or neuromuscular junction disorders (e.g., myasthenia gravis or Lambert-Eaton syndrome) should be monitored particularly closely when given botulinum toxin. Patients with neuromuscular disorders may be at increased risk of clinically significant effects including severe dysphagia and respiratory compromise from typical doses of Dysport.
Human Albumin and Transmission of Viral Diseases
This product contains albumin, a derivative of human blood. Based on effective donor screening and product manufacturing processes, it carries an extremely remote risk for transmission of viral diseases and variant Creutzfeldt-Jakob disease (vCJD). There is a theoretical risk for transmission of Creutzfeldt-Jakob disease (CJD), but if that risk actually exists, the risk of transmission would also be considered extremely remote. No cases of transmission of viral diseases, CJD, or vCJD have ever been identified for licensed albumin or albumin contained in other licensed products.
Intradermal Immune Reaction
The possibility of an immune reaction when injected intradermally is unknown. The safety of Dysport for the treatment of hyperhidrosis has not been established. Dysport is approved only for intramuscular injection.
Adults with lower limb spasticity (≥5%): falls, muscular weakness, and pain in extremity and with upper limb spasticity (≥4%): muscular weakness.
Pediatric patients with lower limb spasticity (≥10%): nasopharyngitis, cough and pyrexia and with upper limb spasticity (≥10%): upper respiratory tract infection and pharyngitis.
Adults with cervical dystonia (≥5%): muscular weakness, dysphagia, dry mouth, injection site discomfort, fatigue, headache, musculoskeletal pain, dysphonia, injection site pain, and eye disorders.
Co-administration of Dysport and aminoglycosides or other agents interfering with neuromuscular transmission (e.g., curare-like agents), or muscle relaxants, should be observed closely because the effect of botulinum toxin may be potentiated. Use of anticholinergic drugs after administration of Dysport may potentiate systemic anticholinergic effects, such as blurred vision. The effect of administering different botulinum neurotoxins at the same time or within several months of each other is unknown. Excessive weakness may be exacerbated by another administration of botulinum toxin prior to the resolution of the effects of a previously administered botulinum toxin. Excessive weakness may also be exaggerated by administration of a muscle relaxant before or after administration of Dysport.
There are no adequate and well-controlled studies in pregnant women. Dysport should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Based on animal data, Dysport may cause fetal harm.
The safety and effectiveness of Dysport injected into proximal muscles of the lower limb for the treatment of spasticity in pediatric patients has not been established. Based on animal data Dysport may cause atrophy of injected and adjacent muscles; decreased bone growth, length, and mineral content; delayed sexual maturation; and decreased fertility.
In general, elderly patients should be observed to evaluate their tolerability of Dysport, due to the greater frequency of concomitant disease and other drug therapy. Subjects aged 65 years and over who were treated with Dysport for lower limb spasticity reported a greater percentage of fall and asthenia as compared to those younger (10% vs. 6% and 4% vs. 2%, respectively).
To report SUSPECTED ADVERSE REACTIONS or product complaints, contact Ipsen at 1-855-463-5127. You may also report SUSPECTED ADVERSE REACTIONS to the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Dysport® (abobotulinumtoxinA) for injection is indicated for the treatment of:
Please see full Prescribing Information, including Boxed Warning and Medication Guide.