ARE YOU A HEALTHCARE PROFESSIONAL?
This site is intended for US healthcare professionals only.
By clicking YES, you attest that you are a healthcare professional licensed in the US.

When stiffness returns too early, the struggle resumes... Use Dysport for symptom* relief that lasts between injections.
*Symptoms of spasticity can include abnormal increase in muscle tone and muscle spasm.

In an international online survey—Patients Living With Spasticity*— almost a quarter of respondents treated with BoNT-A reported a response of less than 3 months5
*This was a global Internet-based survey, designed in collaboration with the World Federation for NeuroRehabilitation. Data were collected in 29 countries over 13 months from 281 patients diagnosed with spasticity (only inclusion/exclusion criteria; 204 respondents (73%) had been treated with BoNT injections) and encourage to participate by their physician. The survey consisted of multiple-choice questions and was designed to be self-completed by patients and anonymous.5
Duration of FDA approval is not intended to imply superiority in efficacy or safety of Dysport
The majority of patients in the clinical studies were retreated between 12 and 16 weeks; however, some patients had a longer duration of response
Dysport is FDA approved for the treatment of spasticity in patients aged 2 years and older
The efficacy and safety of Dysport were evaluated in a randomized, multicenter, double-blind, placebo-controlled study in 238 adults with upper limb spasticity.
The co-primary efficacy endpoints were mean change in Modified Ashworth Scale (MAS) score in the primary target muscle group (PTMG) (elbow, wrist, or finger flexors) and Physician’s Global Assessment (PGA) of response to treatment between baseline and week 4. MAS score at baseline (mean [SD]): placebo, 3.9 (+/–0.4); Dysport 500 Units, 3.9 (+/–0.5); Dysport 1000 Units, 3.9 (+/–0.4).
Follow-up assessments occurred at weeks 1, 4, and 12; follow-up visits were also permitted at weeks 16, 20, and 24 as needed for retreatment. After 3 months of on-study treatment, patients were given the opportunity to continue open-label treatment with Dysport for up to 5 additional treatment cycles.
Study participants included both botulinum toxin treatment-naïve and -experienced patients
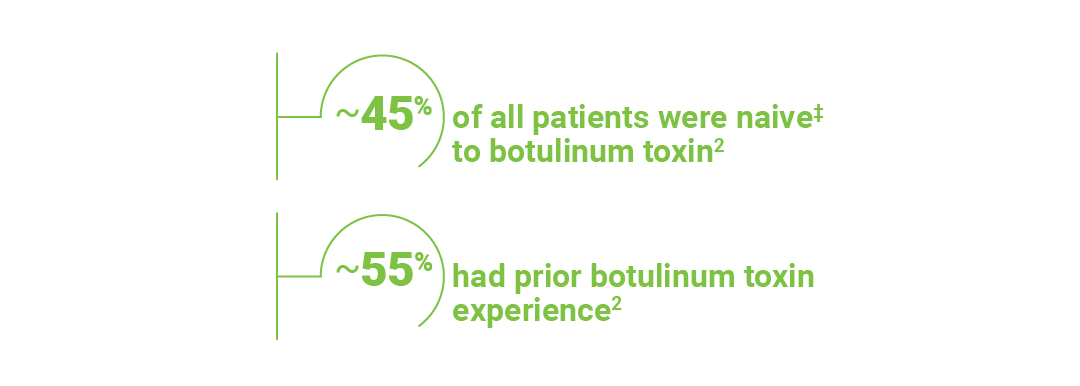
‡Defined as a study participant who had never received any botulinum toxin in the affected upper limb.
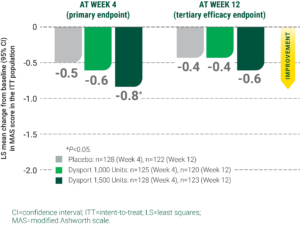
Reduction from baseline in muscle tone as measured by Modified Ashworth Scale (MAS) at week 41

Week 12 results may represent chance findings, as multiplicity adjustments were not applied; interpret appropriately.
Reduction in muscle tone was seen as early as week 1†
†Calculations were based on the number of patients responding at each week divided by the total number of patients at week 4.
Physicians reported a significant (P≤0.05) improvement in response to treatment in patients receiving either dose of Dysport at week 4, as assessed by the Physician’s Global Assessment (PGA) of response to treatment (co-primary efficacy endpoint)
Most commonly observed adverse reactions (≥4%) were muscular weakness

*Patients who remained in the study after week 12 were permitted additional discretionary follow-up at week 16, week 20, and week 24 to assess eligibility for retreatment.
Time to retreatment was not the primary endpoint
In the pivotal trial for adult spasticity, need for retreatment was determined by:
Investigator discretion based on efficacy and safety criteria, determined need for retreatment for patients demonstrating a decrease from baseline of ≥1 grade in MAS score and/or improvement in PGA [ie, a score ≥+1]
Some patients in clinical studies of spasticity had a longer duration of response, ie, 20 weeks
Repeat Dysport treatment should be administered no sooner than 12 weeks after the previous injection
Efficacy-AULS
In the treatment of adults patients with spasticity, start Dysport for lasting symptom relief1
The majority of patients in the clinical studies were retreated between 12 and 16 weeks; however, some patients had a longer duration of response
Dysport is FDA approved for the treatment of spasticity in patients aged 2 years and older
The efficacy of Dysport was evaluated in a randomized, multicenter, double-blind, placebo-controlled study in 381 adults with lower limb spasticity.
The primary efficacy endpoint was muscle tone assessed by LS mean change from baseline in Modified Ashworth Scale (MAS) score at the affected ankle joint at week 4. MAS score at baseline (mean [SD]): placebo, 3.9 (+/–0.5); Dysport 1000 Units, 3.8 (+/–0.5); Dysport 1,500 Units, 3.7 (+/–0.5).
Follow-up assessments occurred at weeks 1, 4, and 12; follow-up visits were also permitted at weeks 16, 20, and 24 as needed for retreatment. After 3 months of on-study treatment, patients were given the opportunity to continue open-label treatment with Dysport.
Study participants included both botulinum toxin treatment-naïve and -experienced patients
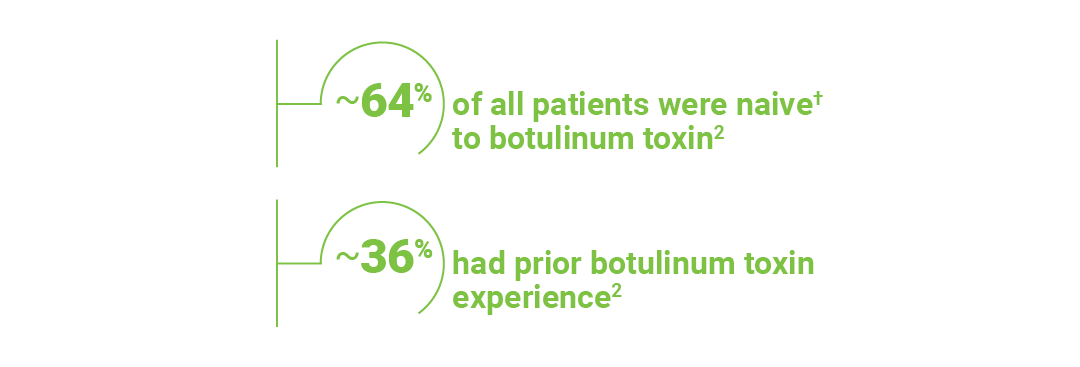
†Defined as a study participant who had never received botulinum toxin in the affected lower limb.
Most commonly observed adverse reactions (≥5%) were falls, muscular weakness, and pain in extremity
Week 12 results may represent chance findings, as multiplicity adjustments were not applied; interpret appropriately.

Time to retreatment was not the primary endpoint
In the pivotal trial for adult spasticity, need for retreatment was determined by:
Investigator discretion based on efficacy and safety criteria, determined need for retreatment for patients demonstrating a decrease from baseline of ≥1 grade in MAS score and/or improvement in PGA [ie, a score ≥+1]
Some patients in clinical studies of spasticity had a longer duration of response, ie, 20 weeks
Repeat Dysport treatment should be administered no sooner than 12 weeks after the previous injection
Patients who remained in the study after week 12 were permitted additional discretionary follow-up at week 16, week 20, and week 24 to assess eligibility for retreatment.
Efficacy-ALLS
Register for Doctor Locator when you sign up for C.L.I.M.B.®
See eligibility criteria at www.CLIMB-training.com
The C.L.I.M.B. educational learning platform is a multitier learning continuum designed to accommodate physicians new to and experienced with botulinum toxin therapy. This educational curriculum is designed to help physicians across all levels improve their clinical skills involving the appropriate use of Dysport. Visit www.CLIMB-training.com to learn more!

Register
Postmarketing reports indicate that the effects of Dysport and all botulinum toxin products may spread from the area of injection to produce symptoms consistent with botulinum toxin effects. These may include asthenia, generalized muscle weakness, diplopia, blurred vision, ptosis, dysphagia, dysphonia, dysarthria, urinary incontinence, and breathing difficulties. These symptoms have been reported hours to weeks after injection. Swallowing and breathing difficulties can be life threatening and there have been reports of death. The risk of symptoms is probably greatest in children treated for spasticity, but symptoms can also occur in adults treated for spasticity and other conditions, particularly in those patients who have underlying conditions that would predispose them to these symptoms. In unapproved uses and in approved indications, cases of spread of effect have been reported at doses comparable to or lower than the maximum recommended total dose.
Dysport is contraindicated in patients with known hypersensitivity to any botulinum toxin products, cow’s milk protein, components in the formulation or infection at the injection site(s). Serious hypersensitivity reactions including anaphylaxis, serum sickness, urticaria, soft tissue edema, and dyspnea have been reported. If such a reaction occurs, discontinue Dysport and institute appropriate medical therapy immediately.
Lack of Interchangeability Between Botulinum Toxin Products
The potency Units of Dysport are specific to the preparation and assay method utilized. They are not interchangeable with other preparations of botulinum toxin products, and, therefore, units of biological activity of Dysport cannot be compared to or converted into units of any other botulinum toxin products assessed with any other specific assay method.
Dysphagia and Breathing Difficulties
Treatment with Dysport and other botulinum toxin products can result in swallowing or breathing difficulties. Patients with pre-existing swallowing or breathing difficulties may be more susceptible to these complications. In most cases, this is a consequence of weakening of muscles in the area of injection that are involved in breathing or swallowing. When distant side effects occur, additional respiratory muscles may be involved. Deaths as a complication of severe dysphagia have been reported after treatment with botulinum toxin. Dysphagia may persist for several weeks, and require use of a feeding tube to maintain adequate nutrition and hydration. Aspiration may result from severe dysphagia and is a particular risk when treating patients in whom swallowing or respiratory function is already compromised. Patients treated with botulinum toxin may require immediate medical attention should they develop problems with swallowing, speech, or respiratory disorders. These reactions can occur within hours to weeks after injection with botulinum toxin.
Pre-existing Neuromuscular Disorders
Individuals with peripheral motor neuropathic diseases, amyotrophic lateral sclerosis, or neuromuscular junction disorders (e.g., myasthenia gravis or Lambert-Eaton syndrome) should be monitored particularly closely when given botulinum toxin. Patients with neuromuscular disorders may be at increased risk of clinically significant effects including severe dysphagia and respiratory compromise from typical doses of Dysport.
Human Albumin and Transmission of Viral Diseases
This product contains albumin, a derivative of human blood. Based on effective donor screening and product manufacturing processes, it carries an extremely remote risk for transmission of viral diseases and variant Creutzfeldt-Jakob disease (vCJD). There is a theoretical risk for transmission of Creutzfeldt-Jakob disease (CJD), but if that risk actually exists, the risk of transmission would also be considered extremely remote. No cases of transmission of viral diseases, CJD, or vCJD have ever been identified for licensed albumin or albumin contained in other licensed products.
Intradermal Immune Reaction
The possibility of an immune reaction when injected intradermally is unknown. The safety of Dysport for the treatment of hyperhidrosis has not been established. Dysport is approved only for intramuscular injection.
Adults with lower limb spasticity (≥5%): falls, muscular weakness, and pain in extremity and with upper limb spasticity (≥4%): muscular weakness.
Pediatric patients with lower limb spasticity (≥10%): nasopharyngitis, cough and pyrexia and with upper limb spasticity (≥10%): upper respiratory tract infection and pharyngitis.
Adults with cervical dystonia (≥5%): muscular weakness, dysphagia, dry mouth, injection site discomfort, fatigue, headache, musculoskeletal pain, dysphonia, injection site pain, and eye disorders.
Co-administration of Dysport and aminoglycosides or other agents interfering with neuromuscular transmission (e.g., curare-like agents), or muscle relaxants, should be observed closely because the effect of botulinum toxin may be potentiated. Use of anticholinergic drugs after administration of Dysport may potentiate systemic anticholinergic effects, such as blurred vision. The effect of administering different botulinum neurotoxins at the same time or within several months of each other is unknown. Excessive weakness may be exacerbated by another administration of botulinum toxin prior to the resolution of the effects of a previously administered botulinum toxin. Excessive weakness may also be exaggerated by administration of a muscle relaxant before or after administration of Dysport.
There are no adequate and well-controlled studies in pregnant women. Dysport should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Based on animal data, Dysport may cause fetal harm.
The safety and effectiveness of Dysport injected into proximal muscles of the lower limb for the treatment of spasticity in pediatric patients has not been established. Based on animal data Dysport may cause atrophy of injected and adjacent muscles; decreased bone growth, length, and mineral content; delayed sexual maturation; and decreased fertility.
In general, elderly patients should be observed to evaluate their tolerability of Dysport, due to the greater frequency of concomitant disease and other drug therapy. Subjects aged 65 years and over who were treated with Dysport for lower limb spasticity reported a greater percentage of fall and asthenia as compared to those younger (10% vs. 6% and 4% vs. 2%, respectively).
To report SUSPECTED ADVERSE REACTIONS or product complaints, contact Ipsen at 1-855-463-5127. You may also report SUSPECTED ADVERSE REACTIONS to the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Dysport® (abobotulinumtoxinA) for injection is indicated for the treatment of:
Please see full Prescribing Information, including Boxed Warning and Medication Guide.